Many doctors and laboratories don't have the resources to comply with the Food and Drug Administration’s final rule on the regulation of laboratory developed tests and will likely scale back the number of tests they perform, experts from the American Medical Association and other healthcare groups warned at a meeting last week.
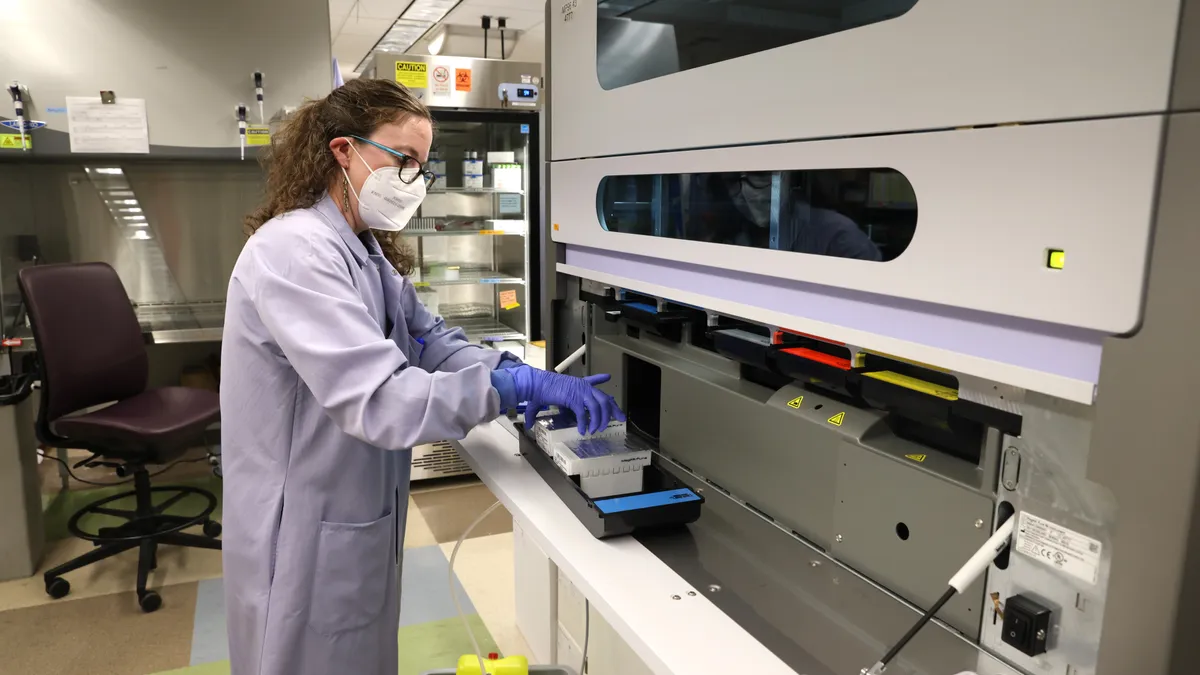
Clinical labs are now assessing the staffing and financial burdens they face as a result of the rule, Octavia Peck Palmer, president of the Association for Diagnostics & Laboratory Medicine, said during a July 30 panel discussion at the group’s annual meeting.
“ADLM believes that if the ruling remains unchanged, it will severely reduce patient access to essential testing,” Peck Palmer said.
The rule, released April 29 and published May 6 in the Federal Register, amends FDA regulations to make clear that in vitro diagnostics, including those developed by a lab, are medical devices under the Federal Food, Drug, and Cosmetic Act. The agency is stepping up regulation of LDTs because it contends some of the tests can be inaccurate or of low quality, putting patients at risk.
In May, the American Clinical Laboratory Association filed a lawsuit challenging the FDA’s authority to regulate LDTs as medical devices, placing the future of the regulation into question.
The ADLM sees the final rule as duplicative, because LDTs are already regulated by the Centers for Medicare and Medicaid Services. The FDA has said the CMS does not have the expertise to oversee tests that have become more complex as diagnostics technology has evolved.
Experts on the ADLM panel said the FDA’s expanded oversight could harm patients by significantly delaying diagnoses and care.
“LDTs allow for physicians and laboratory professionals to diagnose and to treat when there is evidence for their use, and FDA approval is far too slow for the rapidly evolving rate of diagnostic medicine,” said Geoff Hollett, senior policy analyst at the AMA.
Hollett said doctors are now struggling with compliance and whether the new policy will decrease availability and reimbursement of certain tests.
“When we're talking about LDTs and our membership, the main theme that comes up over and over and over again is uncertainty — one of the worst words that can come up in the clinic,” Hollett said. “Any time those questions creep into the physician's head, that means that there will be abstention.”
The AMA represents primary care doctors who rely on LDTs to make initial diagnoses, specialists who use the tests to guide care, and pathologists who perform and analyze tests. Some physicians will have the resources to figure out and navigate the rule, said Hollett, but many will not.
“That means that tests will not be offered, patient care will get worse, and practices will close,” Hollett said.
A mother’s journey
For Sarah Braswell, an LDT performed after the birth of her daughter, Olivia, confirmed a diagnosis of Down syndrome.
Further testing identified related medical conditions, leading to multiple therapies for Olivia, now 7 years old, and services that support the family. A sleep apnea diagnosis, for example, meant Olivia qualified for a medical day care that allowed Braswell to hold a job in addition to caring for her daughter.
The mother of two now uses her knowledge of LDTs to help others.
“As an advocate, I share with other special needs families, especially Down syndrome families, what tests are available and what they should look into,” Braswell said.
LDTs play an especially critical role in children’s medical care, said Meghan Delaney, chief of pathology and lab medicine at Children's National Hospital in Washington, D.C. She explained that childhood diseases often fall into the category of a rare disease for which there is no FDA-approved test on the market.
“LDTs fill this gap because there are no other tests available to monitor and diagnose them,” Delaney said. “Children have often been left behind in the development of new pharmaceuticals, which are usually developed for adults, and the same situation exists for laboratory tests due to small markets and the highly specialized nature of pediatric disease.”
Delaney vouched for the accuracy of LDTs. “In my experience, in my years of running laboratories in pediatric hospitals, there's no difference in how these tests perform,” Delaney said. “They're accurate, and they're effective for our patients and for our physicians.”
With the ACLA’s lawsuit, the future of the regulation is now up to a federal court. Some legal experts also think the Supreme Court’s recent decision to overturn the Chevron deference doctrine will make it easier for litigation challenging federal agency regulations such as the LDT rule to succeed.
Dennis Dietzen, professor of pathology and immunology at Washington University School of Medicine in St. Louis, said he is hopeful the FDA’s final rule on LDTs will be nullified. The regulation is being phased in over four years.
“The problem is, we can’t pretend like it’s going away,” Dietzen said. “So we still have to prepare ourselves for what might come.”