The first quarter of 2024 was dominated by two events for health insurers: turbulence in Medicare Advantage and the cyberattack on claims clearinghouse giant Change Healthcare. Both created significant uncertainty coming into the quarter, with investors braced for the worst.
But while the former caused profits for a number of insurers to plummet, the latter turned out to be a nothingburger for payers’ bottom lines — even, arguably, for UnitedHealth, Change’s parent company.
Insurers doled out other interesting nuggets during calls with investors this spring, including how a CMS final rule regarding dual-eligible individuals could be a major growth driver for Medicaid insurers and updates on state Medicaid contracts up for grabs.
Here are the biggest takeaways from the quarter.
Change Healthcare: not a bang but a whimper
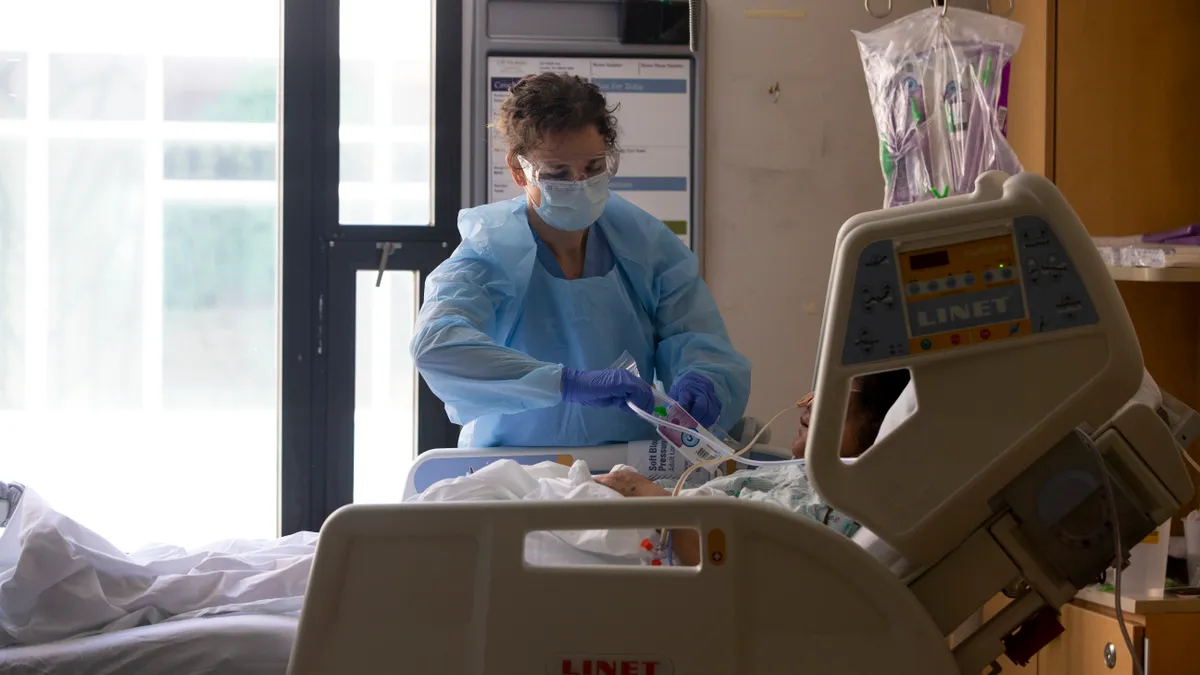
In February, the healthcare industry was rocked by a cyberattack on Change Healthcare, UnitedHealth’s massive payments processor. After Change took its systems offline following the breach, reimbursement to providers and pharmacies ground to a halt, threatening many small businesses and leading UnitedHealth to stand up a loan program amid intense public, legal and governmental pressure.
UnitedHealth CEO Andrew Witty was summoned to the Hill earlier this month amid the public fallout and was grilled by Congress over the breach. Lawmakers also took aim at UnitedHealth’s size and whether it was stifling healthcare competition, a criticism Witty attempted to head off on the insurer’s first-quarter call with investors.
Following the attack, “we were able to bring to bear the substantial resources of UnitedHealth Group to drive the recovery and begin to mitigate the impact — resources which a standalone Change Healthcare would not have had access to on its own,” Witty said.
Witty also described UnitedHealth as a “comparatively small part of the $5 trillion U.S. health system.” That’s despite UnitedHealth being the largest healthcare company in the U.S., with businesses in health insurance, pharmacy benefits, physician practices, banking and more. The company is currently facing an antitrust investigation by the Justice Department, which has grown more concerned about monopoly power in healthcare.
In stark contrast to the cyberattack’s fallout on providers, insurers emerged from the first quarter generally unphased by the breach. That arguably applies to UnitedHealth, too — the company expects up to $1.6 billion in costs this year as a result of the attack, a drop in the water of its $372 billion in annual revenue. UnitedHealth also doesn’t expect the attack to materially impact its 2024 earnings.
As for its peers, “we were not significantly impacted by this,” Elevance CEO Gail Boudreaux told investors in April.
Some insurers did experience a minor increase in operating expenses. But the biggest effect of the attack was that Change taking its systems down made it harder for insurers to predict how much they might have to spend on members’ medical costs.
As a result, major payers pulled hundreds of millions of dollars into reserves to account for claims lodged in the quarter that they had yet to receive.
However, executives assured investors they were confident about the adequacy of those reserves, and that the brunt of delayed claims came in before the quarter’s end.
“By the time we closed the quarter, the impact was very modest,” Centene CEO Sarah London told analysts on the insurer’s April call.
MA utilization catches some flat-footed
Payers continued to jostle with a dogged increase in medical spend as more seniors in Medicare Advantage plans seek out healthcare following the COVID-19 pandemic. Utilization started to tick up early last year and remained elevated in the quarter, reflected in outpatient services like radiology and cardiovascular procedures for Elevance, or mental health and medical pharmacy for CVS, for example.
Inpatient care has risen too, which Centene, Humana, Elevance and CVS noted. The trend is concerning for insurers given hospital services are more expensive to cover. Some payers blamed the “two-midnight rule,” which requires them to cover an inpatient admission if the patient is expected to require hospital care for at least two midnights.
All MA insurers said their members were using more care. But some planned adequately for the increase in utilization, including Elevance, UnitedHealth and Cigna, which said they were comfortable with their pricing and benefit designs for 2024. Elevance, for example, saw its net profit rise 13% year over year because of how much it increased premiums on its members.
Others — Humana and CVS — appeared to have been caught unprepared.
Humana’s net income fell to $741 million in the quarter from $1.2 billion in the same time last year because of surging medical expenses. The insurer, the second largest MA payer after UnitedHealth, even pulled its profit outlook for 2025, citing turbulence in MA.
CVS similarly blamed utilization pressures after its first-quarter net income fell to $1.1 billion, roughly half as much as the insurer brought in during the same time last year. The results caused CVS’ stock to experience its largest single-day loss since 2009, and prompted a downgrade at investment bank TD Cowen.
Importantly, insurers are still notching profits — just not as high as they would like, and not enough to satiate Wall Street’s demand for growth in MA, a program that’s historically brought in significant earnings.
The key questions coming out of the first quarter are, “Will medical cost trends moderate in 2024? If so when and by how much,” and “who benefits most?” wrote TD Cowen analyst Gary Taylor in a note following the quarter.
Humana, CVS paid out significantly more in premiums; expect that to continue
Lower 2025 payment rates than insurers hoped from regulators in Washington looking to crack down on bad actors in the privately run Medicare program aren’t helping, either.
Insurance executives voiced their disapproval during quarterly calls. Elevance’s Boudreaux said she was “disappointed” in the rates, while CVS CEO Karen Lynch called them “insufficient” and a “significant added disruption” in the program.
In light of the challenges, insurers plan to focus on profits over growth, taking actions like cutting benefits, raising premiums or even exiting markets.
UnitedHealth’s Witty said the 2025 rate notice, while “a little disappointing,” is unlikely to change how UnitedHealth is approaching its preparations for next year.
Others said they’ll have to double down on cuts as a result.
The rates “will require larger benefit reductions to achieve stable margins,” Humana CFO Susan Diamond said.
Cowen’s Taylor noted all major MA insurers will likely earn “materially below” target margins this year, and “will be compelled to cut supplemental benefits materially” for 2025. That could reshape current MA market share.
Insurers are finalizing 2025 bids now, and will submit them to the CMS in early June.
Medicaid unwinding cools down as contracts heat up
MA isn’t the only source of turbulence for insurers: Medicaid redeterminations, the process wherein states recheck their beneficiaries’ eligibility for the safety-net program, have been ongoing since last spring.
Millions of Americans have been kicked off the coverage due to redeterminations, raising concerns that the acuity of payers’ membership pools may no longer match what they’re being reimbursed by states.
Though insurers reassured investors that rates have remained actuarially sound, a mismatch between rates and acuity drove up medical spend for Centene and CVS in the quarter. Executives for those payers said they’re talking with states about adjusting rates.
Meanwhile, for many payers, membership gains in the Affordable Care Act marketplaces, along with a steady rate of “rejoiners” — people returning to Medicaid after being improperly removed from the program — have offset the worst of Medicaid losses.
The general sense on first-quarter calls was a looming return to business as usual, given redeterminations are roughly 90% complete, according to Centene, Molina and Elevance.
However, some payers were less than pleased about recent Medicaid contract awards in Florida, Michigan, Virginia and Texas.
Molina lost the Florida and Virginia contracts, which is expected to cost the company $500 million in revenue this year. Meanwhile, Centene lost in Texas and UnitedHealthcare lost in Florida.
Molina and Centene said in first-quarter calls they plan to challenge the decisions, while UnitedHealthcare didn’t say outright but suggested it might protest.
Along with challenging existing losses, insurers are also gearing up to fight for upcoming contracts. An estimated $60 billion in premiums is up for bid over the next three years, according to Molina CEO Joe Zubretsky.
CMS opens D-SNP door
Centene and Molina, both large Medicaid insurers, told investors they have a significant growth opportunity thanks to a new CMS rule finalized in April meant to streamline continuity of care for people covered by both Medicare and Medicaid.
Currently many dual-eligible members receive Medicaid and Medicare benefits from two different insurers. The rule essentially will move those unaligned members to the Dual Special Needs Plan (D-SNP) plan run by their Medicaid insurer.
As a result, having a broad Medicaid footprint will be a catalyst for MA growth, especially as the D-SNP population is forecasted to grow, insurance executives said.
“The strategic link between Medicare and Medicaid has only become more explicit,” said Centene’s London. “By the end of the decade, a Medicaid footprint will be a prerequisite to D-SNP growth.”
Molina executives said the rule should help the insurer reach its mid-single digit target margins in Medicare — a higher target than some of its competitors, given it has a high percentage of dual-eligible members already.
Those members tend to be higher acuity, so the government pays insurers more to manage their care.
“We like the D-SNP business, not only because it can produce excellent profits, but monetizing our Medicaid footprint for dual-eligible share over time is going to be a significant growth catalyst for us,” said Molina’s Zubretsky.